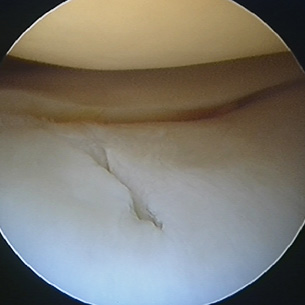
Large split found in the articular cartilage (gristle) of the knee at arthroscopy.
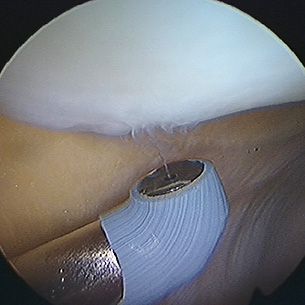
A radiofrequency probe being used to remove a small area of arthritic damage on the back of the kneecap (patella)
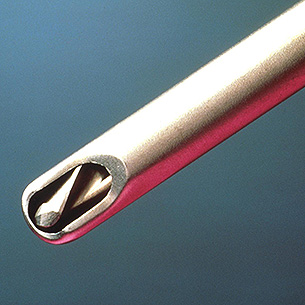
An arthroscopic shaver blade. The cutter rotates very fast (8000 rpm) within the tube, while simultaneous suction removes the cut debris.
The fact an operation is performed through small keyhole incisions does not mean it is simple. Indeed, there are some surgeons who, even to this day, find it difficult to master the art of endoscopic surgery.
Arthroscopy may be performed under local or general anaesthetic and is normally a daycase operation. That is, admission, operation and discharge all take place on the same day. For those coming from further afield, it may be necessary for admission to be the day before surgery, or discharge to be the day after.
Once in the operating theatre, the patient's skin is prepared with a special antiseptic solution in order to kill the bacteria that live as commensals on all our skins. The leg is then draped with sterile drapes to seal off the operating area from the rest of the body and surgical staff who are not playing a direct part in the procedure.
Then, with a small knife, the surgeon makes a tiny incision ('stab' incision) just to the outer side of the patellar tendon (kneecap tendon). Through this incision the arthroscope is introduced, using a series of trocars through a metal cannula, no more than 5 millimetres in diameter. Once the arthroscope has been inserted, a further stab incision is made on the other side of the patellar tendon and through this portal an arthroscopy hook is inserted. The hook is an important instrument. It allows the surgeon to probe suspicious areas, to feel the strength of ligaments, or to reposition loose bodies so they can be more easily retrieved.
The surgeon then makes a thorough inspection of the knee joint, looking into every crevice possible, and then decides on the appropriate operation. This may be a meniscectomy (cartilage removal), or debridement ('clean-out' operation), ligament reconstruction, or any number of alternatives. The hook is then removed and more definitive surgical instruments inserted. These instruments may be manually operated, radiofrequency, laser-driven, or powered. The so-called 'power shavers' comprise rapidly rotating cutting blades, often with a diameter of less than 3.5 millimetres, that can both cut and suck at the same time. All the cut material is thus rapidly and automatically removed from the joint.
Once surgery is complete, the instruments and arthroscope are removed and the small portal wounds may either be left as they are to heal naturally or may be sutured, stapled, taped, or even glued!
Following discharge it is common for patients to feel discomfort, though not to a great level, for about four weeks. Those for whom osteoarthritis (OA) is the diagnosis can sometimes feel discomfort for longer. In a few cases of OA, pain can persist for several months. For the majority, however, after this four-week period, they are back to reasonable normality, although it can sometimes be up to a month for symptoms to fully settle.
It is common for the knee to be slightly swollen during this period. Sports can be resumed to a limited extent one month after surgery and physiotherapy is frequently encouraged for at least this period. However, it can be anything up to three months following arthroscopy before a knee has fully settled after a knee arthroscopy. On occasion it may take even longer to resolve.
