
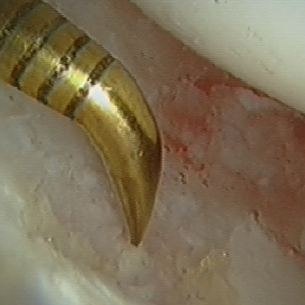
An arthroscopic probe (metal hook) gently pressing on the diseased cartilage in the hip to elicit the ‘wave sign’- a bubble of cartilage forming, which confirms that the cartilage has delaminated and lifted off from the underlying bone. This is potentially a precursor to advanced arthritis.
Cartilage defect in hip joint on acetabulum (cup) where microfracture are being undertaken for marrow stimulation.
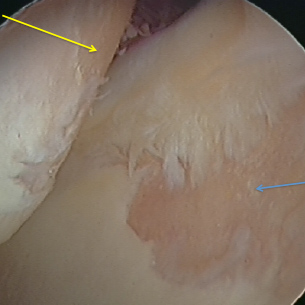
Significant cartilage damage in the hip joint. The yellow arrow is pointing to the damage on the femoral head (ball) and the blue arrow to the acetabulum (socket). Note the pink edges of bare bone adjoining the white edge of the remaining cartilage.

Key-hole surgery (arthroscopy) of the hip underway. Surgeon uses a variety of instruments, techniques and gadgets including X-yay flourscopy and modern fibreoptics to undertake the surgery safely and effectively.
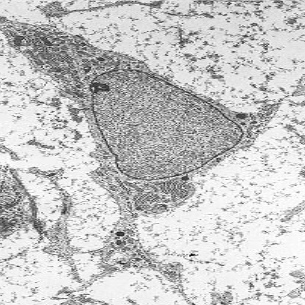
Mesenchymal Stem Cell By Robert M. Hunt
(Own work) [GFDL (http://www.gnu.org/copyleft/fdl.html)
or CC-BY-3.0 (http://creativecommons.org/licenses/by/3.0)], via Wikimedia Commons
What is biological therapy?
Biological therapy in orthopaedics, also known as orthobiologics, comes in various forms. Examples include autologous (patient’s own) blood injection, platelet-rich plasma (PRP) and cell therapy. Cell therapy exists in different forms, too. These might include bone marrow aspirate concentrate (BMAC), adipose tissue (fat) harvested cells, autologous chondrocyte implantation (ACI) and even microfracture, which is a basic version of biological therapy and possibly the most widely performed. Stem cell therapy is also a form of biological therapy and is widely discussed, debated and analysed in modern medicine and the scientific literature. Let us have a closer look at them.
What are stem cells?
Stem cells are perhaps Nature’s best-kept secret. These cells, which are found in multicellular organisms, such as humans, not only have the ability to divide (mitosis) but also to form various structures such as cartilage, bone and many more. The process is called ‘differentiation’.
What types of stem cell are there?
There are two basic forms of stem cell - the embryonic stem cell and adult stem cell. Adult stem cells, which are also known as mesenchymal stem cells or MSCs are of great interest to researchers, scientists and surgeons alike. MSCs are free of the controversy that surrounds the embryonic stem cells and yet may have the potential to form new tissues. MSCs can be found at various locations in the body including bone marrow, adipose tissue (fat) and peripheral blood.
Where do the cells come from that are used in biological therapy?
At the Villar Bajwa Practice we use the cells from bone marrow concentrate, or sometimes from peripheral blood. We know bone marrow to be rich in stem cells, and other cells, too. This can potentially help repair and regenerate tissues such as cartilage and bone more effectively. The cells are harvested autologously (directly from the patient) from bone marrow in the operating theatre at the same time as the arthroscopic surgical procedure (keyhole surgery) is carried out. There is thus no additional risk of disease transmission, rejection or ethical controversy that might exist when using cells from an unrelated donor, or perhaps processed in a facility outside the operating theatre itself. Everything takes place in the operating theatre and under the same anaesthetic. Each of us has a supply of cells including MSCs in various tissues and these can be harvested using specialised techniques and commercially available kits.
Where can cells be used?
By their very nature, cells can be used in a variety of different situations; the aim being to help in the repair and regeneration of damaged tissues and structures. This is being explored in many medical applications. In joint preservation, one role of cells is in the possible management of arthritis of the hip and knee joints. The aim is to help encourage the regeneration of cartilage (gristle). In simple terms, the gristle on the joint surface is the barrier to arthritis. Once this layer is damaged, the joint is likely to progress to frank arthritis, which presents as pain, stiffness and loss of function. Orthopaedic surgeons have not been very successful over the generations in persuading articular cartilage to heal. Cell therapy is one way they are trying to improve on this. The procedure is designed to help preserve the natural hip and knee joint. Results are promising but still very much in their infancy.
Another area of interest for biological therapy in the hip and knee, and this includes cell therapy, is to help with the regeneration of dead bone. In a condition called avascular necrosis, or AVN, there is death of a segment of the bone near the joint. This can sometimes progress onwards to become severe arthritis. Early reports of the use of cells to regenerate bone in AVN are encouraging.
There are many other reasons why cell therapy might be used. These techniques may be relevant to different patients and can be employed as required.
What does the procedure involve?
The procedure is in the form of arthroscopy (keyhole surgery) of the hip or knee. Patients often ask whether cell therapy (BMAC) involves surgery on two separate occasions. For the techniques that we use, only a single operation is normally required. This is generally carried out as a day-case procedure for knee arthroscopy while most hip arthroscopy patients will have a one-night stay in hospital. Once the patient is under general anaesthesia, an aspirate of their blood and/or marrow is taken with a special needle. The bone marrow is concentrated using multiple centrifugations in the operating theatre, and while the patient is still asleep, to concentrate the cell fraction. At the same time the keyhole operation (arthroscopy) is commenced to access the hip or knee joint. The surgeon uses specialist arthroscopy techniques to prepare the tissue bed so that it is ready to receive the BMAC. The harvested cells, alongside a suitable scaffold, are then injected through the same keyholes that are routinely used for the arthroscopy.
What are the side effects?
Any surgical intervention carries a degree of risk and those are explained elsewhere on this website. However, the surgical procedures used for cell therapy are the same as those for routine hip or knee arthroscopy operations (complications of hip and knee arthroscopy). There is a theoretical risk of infection, but this is low and surgery is in any event covered by antibiotic treatment.
What is the evidence for cell therapy?
Cell therapy is a relatively new procedure. However, it has created so much interest worldwide that extensive research has been taking place in this field. Animal and human studies have been published that have suggested a favourable response to cell therapy in hips, knees and even ankles. Our practice routinely collects data on almost all patients who undergo surgical treatment under our care; assessment questionnaires are periodically sent to those who have undergone surgery. This is an invaluable source of information that helps us to inform our patients, publish in the literature, and train others who are interested in the techniques we undertake.
Next Steps – what to do if you think you may benefit from biological therapy?
Insured Patients: Simply visit your GP and ask them to refer you to either Mr Ali Bajwa or Mr Richard Villar of the Villar Bajwa Practice at the Princess Grace Hospital, London. Mr Richard Villar has now retired from operating in the United Kingdom, although still holds clinics, but Mr Bajwa is undertaking surgery frequently. Clinics are held regularly in both Cambridge and London. Your GP will write a letter of referral and then either you or your GP can contact us to arrange your first out-patient appointment on 0207 908 3777.
Self-Pay Patients: To book a consultation, we will require a referral to Mr Bajwa or Mr Villar from your GP or Specialist.
